Heart Failure
Heart (or cardiac) failure is a condition when the heart is unable to pump enough blood to meet the body’s need. It means that either the heart can’t fill with enough blood or pump with enough force, or both. A lot of underlying heart problems can result in heart failure. Pre existing conditions like high blood pressure, coronary artery disease, heart valve diseases like aortic regurgitation gradually weaken the heart leaving it weak and stiff. This reduces the efficiency of the heart pump.
Many conditions that lead to failure cannot be reversed. In some cases the problem maybe treated. Available drugs can be used to improve survival by improving the signs and symptoms of heart failure. Exercise, reducing weight, reducing salt intake, managing stress measures to alter the way one lives help in improving quality of life by reducing fluid buildup. It is important to aggressively prevent or control risk factors. Coronary artery disease, diabetes, high blood pressure, overweight/obesity, high cholesterol levels need to be targeted.
What is Heart failure?
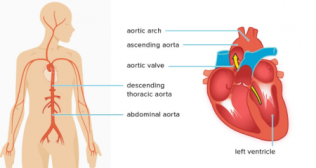
Heart failure occurs as the heart action grows weaker with time due to underlying problems. It can affect the right side, the left side or both of the heart. The left sided failure is more common. The heart being unable to pump oxygen and nutrition enriched blood to the rest of the body. In right sided failure the heart is unable to push the blood into the lungs for oxygen enrichment.
Heart failure is called by different names.
- Congestive heart failure or CHF (when the poor pumping of the heart causes) symptoms)
- Left-sided heart failure
- Right-sided heart failure
- Systolic heart failure (the left ventricle loses its ability to contract vigorously)
- Diastolic heart failure (the left ventricle loses its ability to relax or fill fully)
A combination can be present. While in most cases heart failure progresses over time in certain cases the normal heart maybe suddenly presented with a load that it is unable to handle.
The result of weakened pumping of the heart’s manifests as:
- Blood and fluid building up in the lungs
- Fluid accumulation in the feet, ankles, and legs
- Tiredness and shortness of breath
Incidence
Heart failure is a serious condition. A person aged 40 years or older has a 1 in 5 chance of developing heart failure. Currently, about 5 million Americans are living with heart failure and about 550,000 new cases are diagnosed each year. The number is growing.
African-Americans between the ages of 45 and 64 are 2.5 times more likely to die from heart failure than Caucasians in the same age range. Based on data from the Census Bureau and the Centers for Disease Control and Prevention, it is estimated that there are approximately 700,000 African Americans with heart failure in the United States, and this number is expected to grow to 900,000 by 2010. Between the ages of 45 and 64, African American males have a 70% higher risk for heart failure than Caucasian males. African American females between the ages of 45 and 54 have a 50% greater risk to develop heart failure than Caucasian females.
The incidence of heart failure has risen among the elderly, possibly due to improved survival of coronary disease from better surgical and medical treatments, according to a University of Rochester study. The high prevalence combined with multiple complications from this condition increase health care costs significantly.
Signs and Symptoms
The signs and symptoms of heart failure are a result of the heart being unable to push the blood forward effectively. The blood backs up into or congests the organs and tissues.Some people with heart failure have few complaints. While in those with chronic heart failure (when the congestion occurs slowly over time) the common complaints are:
- General feeling of tiredness or weakness
- Shortness of breath (while exerting oneself or even at rest if severe)
- Reduced ability to exercise
- Persistent cough or wheezing with white or pink blood-tinged phlegm
- Swelling (edema) in legs, ankles and feet
- Swelling of abdomen (ascites)
- Sudden weight gain from fluid retention
- Lack of appetite and nausea
- Difficulty in concentrating or decreased alertness
- Irregular or rapid heartbeat
When the ability of the heart to function is suddenly affected the complaints are similar to those of chronic heart failure but more sudden and severe. Signs and symptoms of acute heart failure may include:
- sudden fluid buildup
- rapid or irregular heartbeat with palpitations
- sudden, severe shortening of breath
- coughing of pink, foamy mucus
- chest pain if due to a heart attack or an aneurysm
Causes of Heart Failure
Heart failure can occur due to many causes. Sometimes the exact cause may not be found. The most common causes of chronic heart failure are:
- Coronary artery disease (narrowing of the blood vessels to the heart) is the commonest cause of heart failure. The narrowing results in reduced blood flow to some areas of the heart chronically depriving them of oxygen rich blood. Over time these areas weaken and pump less actively. Sometimes the blood flow is completely cuts off causing a heart attack. This damages the heart muscle weakening its ability to pump.
- Problems with the heart muscle (cardiomyopathy) can result from infections, alcohol abuse, from chemotherapy drugs or as a result of the toxic effects of drugs like cocaine. Conditions such as lupus or thyroid problems can also damage the heart. When no specific cause can be identified it is called idiopathic dilated cardiomyopathy.
- High blood pressure (hypertension) makes the heart work harder to circulate blood throughout the heart. The heart muscle may become thicker to compensate the extra work it has to do. In some cases the heart enlarges eventually becoming stiff and weak.
- Problems with any of the four heart valves puts load on the heart. The heart has to work harder. The extra work weakens the heart.
- Abnormal heart rhythms (arrhythmias) put extra load on the heart. Over time the heart weakens leading to heart failure. A slow arrhythmia may prevent the heart from getting enough blood to the body leading to heart failure.
- Congenital heart disease (heart defects present at birth) requires the healthy parts of the heart to work harder to compensate.
- Myocarditis indicates an inflammation of the heart muscle. Commonly caused by a virus it can lead to left-sided heart failure.
- Other conditions such as diabetes, severe anemia, sleep apnea, thyroid problems also contribute to heart failure.
Acute heart failure can result from heart attacks, viral infections uses that attack the heart, severe infections, allergic reactions, blood clots in the lungs, use of certain medications or any illness affecting the whole body. These conditions cause the heart’s pumping action to deteriorate suddenly. Acute heart failure is an emergency.
Screening and Diagnosis:
The doctor will take a detailed medical history and perform a physical examination. Blood pressure, chest congestion, abnormal heart sounds can be detected during a physical examination.This is followed up with diagnostic tests .They help diagnose heart failure, determine its underlying cause and guide treatment decisions.
- Blood tests help verify kidney, thyroid function and indicate others. Specific chemical markers like the brain natriuretic peptide (BNP) secreted by the heart when overworked or injured can be detected.
- Chest x-ray images the heart and lungs. An enlarged heart or fluid in the lungs among others can be detected.
- Electrocardiogram (also called EKG or ECG) is a diagnostic tool that records the electrical activity of the heart and helps diagnose heart rhythm abnormalities.
- Echocardiography an important diagnostic test uses sound waves to estimate the pumping ability of the heart and assess the health of the valves & chambers of the heart.
- Coronary Angiography is a diagnostic test uses an injected dye to identify narrowed arteries to the heart (coronary artery disease) that may be a cause of heart failure. The test may include a ventriculogram which determines the strength of the left ventricle and estimates the health of the heart valves.
- The nuclear heart scan (also called Radionuclide Imaging or Radionuclide Ventriculography) uses radioactive tracers (such as technetium or thallium) to outline the heart champers and major blood vessels leading to and from the heart. It shows any damage to the heart muscle and can be used to diagnose heart disease, valve disorders, or heart failure.
- Cardiac Magnetic Resonance Imaging (MRI) and Cardiac Computed Tomography (CT) are new cardiac imaging methods helps take a closer look at the heart and great vessels.
Treatment
Heart failure cannot be cured. It needs lifelong management. Measures can improve the heart’s pumping and improve the signs and symptoms of heart failure.Treatment modalities include changes in the way one lives, medicine and sometimes devices that help the heart beat properly.The importance of an educated diet, alcohol restriction, stopping smoking, regular exercise, weight control, and support groups cannot be stressed enough.
- Prescription medication may include one or a combination of drugs used to treat heart failure like:
- Angiotensin-converting enzyme (ACE) inhibitors help open (dilate) the arteries, lower blood pressure, improve blood flow and reduce the workload on the heart. Some may promote water & salt retention. In some individuals they cause an irritating cough
- Angiotensin II (A-II) receptor blockers (ARBs) have many of the beneficial effects of ACE inhibitors and don’t cause a persistent cough. They offer an alternative for people who can’t tolerate ACE inhibitors.
- Diuretics often called “water pills” make one urinate more often helping to reduce the fluid load. They decrease fluid in the lungs making breathing easier. Diuretics make the body lose potassium and magnesium. Their levels have to be monitored during therapy and a supplementation prescribed if needed.
- Beta blockers slow the heart rate and reduce blood pressure. They may reduce signs and symptoms of heart failure and improve heart function.
- Digoxin (digitalis) helps the heart pump better. It tends to slow the heartbeat. Heart failure symptoms reduce.
- Aldosterone antagonists primarily potassium-sparing diuretics help the heart work better, may reverse scarring of the heart and help people with severe heart failure live longer. The potassium blood levels need close monitoring.
If hospitalized for heart failure symptoms additional medications such as inotropes (dobutamine, milrinone) and intravenous (IV) vasodilators (IV nitroglycerin) maybe given. They relieve symptoms by helping the heart pump better. Supplemental oxygen maybe required. Newer drugs are under study.
Medicines should be taken strictly to prescription.
Surgery and medical devices : Surgery maybe recommended to treat the underlying problem leading to heart failure. Repair or replacement of a damaged heart valve, ‘fixing’ a coronary artery block valve may be advised.
Alternative treatments available are:
- Implantable cardioverter-defibrillator (ICD) is a device implanted under the skin and attached to the heart with small wires. It monitors the heart rhythm. If the heart starts beating at a dangerous rhythm, the ICD shocks it back into normal rhythm. Sometimes a biventricular pacemaker is combined with an ICD for people with severe heart failure.
- Cardiac resynchronization therapy (CRT) or biventricular pacing sends timed electrical impulses to both lower chambers (the left and right ventricles) of the heart synchronizing their pumping making it more efficient and coordinated.
- Heart pumps are mechanical devices, called left ventricular assist devices (LVADs), are implanted into the abdomen and attached to a weakened heart to help it pump. Earlier used only as interim treatment to help keep heart transplant candidates alive while they waited for a donor heart they are now being considered as an alternative to transplantation.
- Individuals suffering from severe heart failure that can’t be helped by either surgery or medications need to have their diseased heart replaced with a healthy donor heart. Heart transplants have dramatically improved the survival and quality of life of people with severe heart failure.
Experimental treatments
The search is on to develop and discover newer treatment modalities to help person’s suffering from heart failure.
Certain experimental treatments are:
- Cardiac wrap surgery is a technique that involves wrapping a failing heart in a mesh bag, helping to prevent further failure. The goal is to prevent a weakened heart from enlarging (dilating) and failing further.
- Ventricular restoration surgery is a technique that can be used to treat heart failure resulting from a heart attack. During surgery the scar tissue in the ventricular muscle caused by heart attack is removed. The remaining healthy tissue is reshaped to restore a more normal elliptical left ventricle shape. Reduced size and reshaping of the left ventricle helps restore normal function to the pumping mechanism.
- Enhanced external counterpulsation (EECP) is a noninvasive technique. Inflatable pressure cuffs placed on the calves, thighs and buttocks are inflated and deflated in sync with the heartbeat. EECP is supposed to increase blood flow back to the heart.