Cardiovascular Disease Management In Covid 19
[caption id="attachment_9854" align="aligncenter" width="572"] Heart Attack, Heart Disease, Heart - Internal Organ, Illness, Research[/caption]
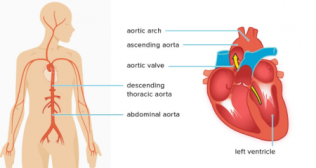
The SARS-CoV 2 causing COVID-19 has reached pandemic levels. It not only causes viral pneumonia but has major implications for the cardiovascular (CV) system. Patients with CV risk factors including male sex, advanced age, diabetes, hypertension and obesity as well as patients with established CV, cerebrovascular disease, rheumatic heart disease and Chagas disease are particularly vulnerable with increased morbidity and mortality when suffering from COVID-19. Apart from arterial and venous thrombotic complications presenting as acute coronary syndromes (ACS) and venous thromboembolism (VTE), myocarditis may worsen heart failure (HF). Moreover, a wide range of arrhythmias has been reported to complicate the course of COVID-19 including potential pro-arrhythmic effects of medical treatment targeted at COVID-19 and associated diseases.
Common cardiac complications in COVID-19 are Hypotension, Myocarditis, Arrhythmias, and sudden cardiac death (SCD). Cardiac patients coming to the ER need to be triaged based on underlying health risks such as hypertension, diabetes, prior cardiovascular or respiratory disease, kidney failure and cancer as part of the process to identify patients with a higher likelihood of developing a severe form of COVID-19 and implement targeted care.
Special attention must be given to ensuring that there are separate facilities in place for dealing with COVID-19 cardiac patients and non-COVID-19 cardiac patients including catheterization.
Management measures:
Continuing treatment with ACE-I and ARBs in patients receiving it for managing high blood pressure. Close monitoring of blood sugar fluctuations: the challenges of management is critical as diabetics are also at high-risk for COVID-19 related mortality, and more vulnerable to viral infections.
Acute coronary syndrome
Cardiologists face particular challenges when caring for patients who present with chest pain or symptoms of acute coronary syndrome (ACS). Because “Troponins” — the substances that are present in the heart muscles and are released in the blood in the event of a heart attack — can be high in patients with COVID-19 who otherwise don’t have heart disease, taking clinical history, performing an electrocardiogram, and measuring troponin levels are some of the first lines of defense. ACS patients should be treated according to established guidelines, with special precautions taken with patients who have high fever and are at a higher risk for developing COVID-19.
Parameters must be defined for types of patient treatment and decisions on procedures that are urgent or can be deferred. A basic necessity is dedicated infrastructure for managing ACS in patients with COVID-19, along with crystal clear information so that suspected or diagnosed COVID-19 patients with ACS know exactly where they can access assistance. Testing for diagnosis of COVID-19 should be available at the same facilities that manage ACS patients.
Invasive procedures like catheterization — should be reserved for critical patients provided that the facility has systems in place for non-transmission of coronavirus during transport and treatment. Patients with stable blood circulation can have pending invasive procedures deferred.
If existing hospitals have cardiac units with more than one catheterization lab, one lab could be designated for management of COVID-19 positive or suspected COVID-19 patients, with the strictest cleaning required after managing each COVID-19 patient.
Oral or surgical treatments to restore blood flow to the heart must also consider risk to medical personnel, staff availability and the number of high-dependency beds in a hospital. Along with risk from viral inflammation, heart patients also face the risk of fatty deposits in the arteries (plaque) that might rupture and medicines such as aspirin and others are a possible therapeutic way forward.
Management measures for ACS patients with COVID-19 emerge according to confirmed and suspected cases.
In confirmed cases of COVID-19:
Patients at low risk of heart attack (STEMI) can be treated to have blood clots dissolved (thrombolysis) while cardiac catheterization should be considered for if thrombolysis is unsuccessful.
Patients at high risk of heart attack would likely need primary Coronary angioplasty instead of thrombolysis but risks to medical staff must be considered in taking this decision, along with availability of appropriately trained lab staff.
Conservative management is a recommended for patients at lowest risk of heart attack (NSTEMI).
In suspected COVID-19 cases infection presenting with ACS:
STEMI patients should receive treatment to dissolve clots (thrombolysis), as with patients who are confirmed as COVID-19 positive.
NSTEMI patients would not have full-blown treatment or invasive procedures but rather, more conservative management, pending test results for COVID-19. Timing is important so that results of COVID-19 tests can be integrated into planning and decision-making for control of infection.
COVID-19 patients can have a very low count in platelets that are responsible for stopping bleeding by helping cells to clot; this becomes a critical consideration in whether or not to perform surgery.
Management measures for myocardial injury in COVID-19 patients:
Current guidelines for the treatment of viral myocarditis should be applied, including the use of standard heart failure therapies and supportive measures. Prednisolone, a steroid, has shown some benefit in a few patients.
COVID-19 infection has been associated with abnormalities in blood clotting. Anticoagulation treatments to stop clotting could be beneficial.
Non COVID Heart patients should continue with Aspirin to prevent micro clots.
Heart failure and COVID-19
Managing heart failure (HF) patients with suspected or confirmed COVID-19 begins with recognizing that respiratory infection is a common trigger of suddenly worsening symptoms– heart failure decompensation. Patients with chronic cardiac conditions, including HF, are predisposed to respiratory infections and to the complications that can occur with signs and symptoms of both cardiac and respiratory conditions overlapping. The high virulence and transmissibility of COVID-19 calls for extraordinary efforts to minimize exposure to both patients and medical staff.
Management measures include:
Stable patients with chronic heart failure (HF) may be followed up via telemedicine as far as possible, with elective procedures deferred. Routine flu vaccination should be considered for patients with chronic HF.
Patients in unstable condition coming to the healthcare facility as well as caregivers at the facility must adhere to the strictest safety measures such as adequate physical distancing, access to, and use of, personal protective equipment (PPE). Adapting infrastructure can entail sectioning off staff, wards and equipment as far as possible, and establishing patient front-facing versus non-patient-facing teams, COVID-19 positive versus negative patients wards to minimize cross-contamination, thorough disinfection of equipment used for patient evaluation, and limiting visitors but using virtual means to communicate with patients’ relatives as much as possible.
Clinical assessment should focus on history and physical examination, isolating patients until the diagnosis of COVID-19 is established or excluded and this may require repeated swab testing.
Standard investigations in the evaluation of HF patients should be considered with a number of caveats that range from conducting bedside assessments, requesting tests that affect management outcome or save lives, and with parameters for carrying out more technical, medical procedures.
Treatment of patients with heart failure and confirmed COVID-19 should include considerations that include, continuation of medical therapies,
The patients with Rheumatic Heart disease, when admitted for acute symptoms need to be treated primarily as other heart failure patients from diverse causes.
Patients requiring cardiac surgeries, if not an emergency, should defer the procedure. If an emergency, a negative Covid report should give a go ahead to the performing surgeon.